Why do Doctors test patellar reflexes....? Because they get a kick out of it
Patella dislocation.
Today we are going to review patella dislocations, one of my favorite orthopedic injuries.
Pt: 15 yo male comes in via EMS for evaluation of a knee injury. Patient was at football practice when he was “tackled weird.”
Exam: Patient holding knee in flexion with a laterally displaced patella.
Don’t get tunnel vision. Assess the joints above and below.
Ensure there is no neurovascular compromise. Check pulses and look for sensory deficits.
Check ROM.
Look for open wounds or soft tissue injuries.
If you suspect a ligamentous injury (i.e. unstable joint) this may be a knee dislocation, which is a whole other can of worms and can be detrimental if missed (i.e. popliteal artery injury).
Xrays not may not be necessary before reduction unless there is question of additional injury or alternative diagnosis.
Management
Spontaneous reduction is common.
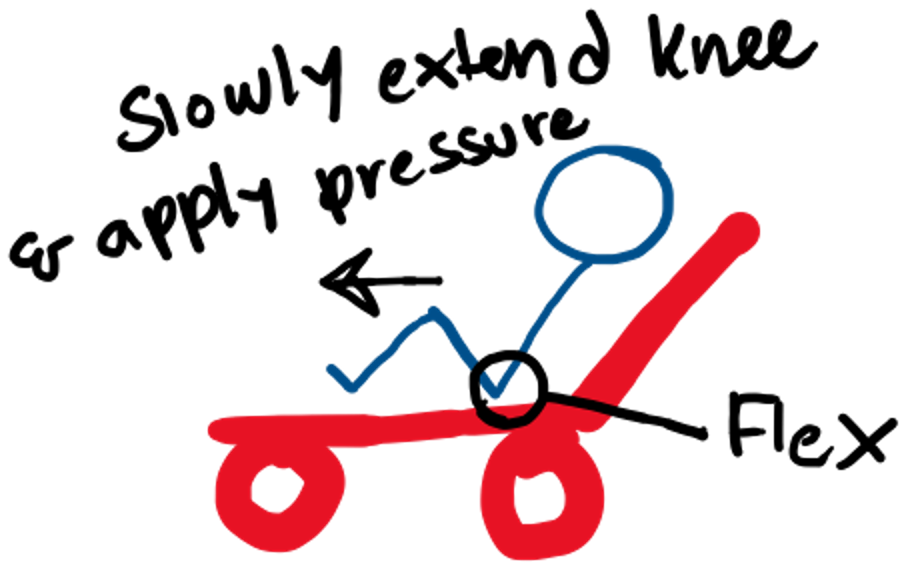
Reduction: With the patient in a semi-fowler position, flex the hip slowly while extending the knee longitudinally along the stretcher and apply pressure to the patella. I often ask for an extra set of hands to help with the reduction.
Assess post reduction neurovascular status and confirm reduction with xray.
Place in knee immobilizer and provide with crutches.
Follow-up: Generally have the patient follow-up with ortho in 2-3 days. Patient will require physiotherapy.
There is limited/conflicting data regarding the role of surgery in patella dislocations in children.
Children under the age of 16 have a high risk of reccurence.